Virtual Care, When and Where You Choose
Get health care quickly with Virtual Urgent Care, Virtual Primary Care, or Message Only Care in the MyMountSinai app
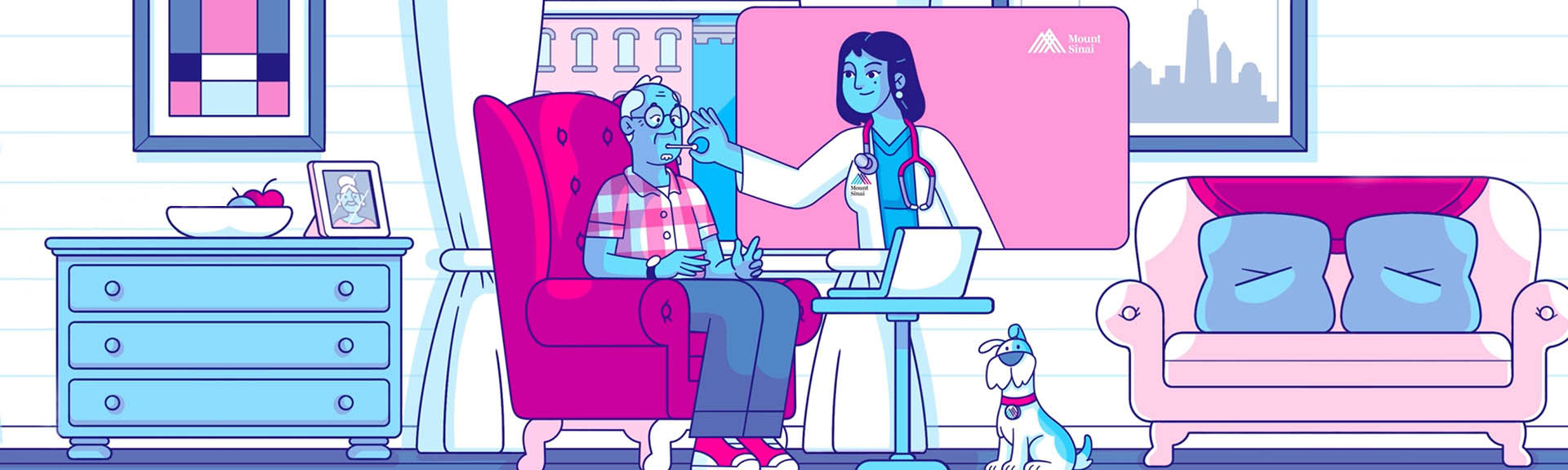
Digital Patient Tools and Resources
See how our expert care is always there

New Center for Refractive Solutions at NYEE
The Center provides the most advanced vision correction services to patients who want to reduce their dependence on eyeglasses or contact lenses—through cataract surgery or corneal refractive procedures such as LASIK.

Virtual Care, When and Where You Choose
Get health care quickly with Virtual Urgent Care, Virtual Primary Care, or Message Only Care in the MyMountSinai app
Digital Patient Tools and Resources
See how our expert care is always there

New Center for Refractive Solutions at NYEE
The Center provides the most advanced vision correction services to patients who want to reduce their dependence on eyeglasses or contact lenses—through cataract surgery or corneal refractive procedures such as LASIK.

Virtual Care, When and Where You Choose
Get health care quickly with Virtual Urgent Care, Virtual Primary Care, or Message Only Care in the MyMountSinai app
Founded in 1820 and now one of the world’s leading facilities for treating diseases of the eyes, ears, nose, and throat, New York Eye and Ear Infirmary of Mount Sinai (NYEE) combines a rich history of specialty care with award-winning clinical excellence in order to serve our community, as well as patients from the Tri-State area, across the nation, and internationally. In addition to our main campus near Union Square, NYEE is growing a network of satellite offices and freestanding ambulatory surgery centers, making access to the newest diagnostic services, advanced treatments, and clinical trials more convenient to our patients’ workplaces and homes.
In addition to providing skilled primary through tertiary care, NYEE is home to breakthrough clinical research that has introduced now widely practiced diagnostic and surgical techniques. Our physicians are also passing the tradition of excellence onto future generations through highly competitive residency programs in ophthalmology and otolaryngology, plus dozens of post-graduate ophthalmology fellowship positions. Through this combination of superb patient care, innovative research, and rigorous education, NYEE is maintaining a leadership position in the fields of ophthalmology, otolaryngology, head and neck surgery, and plastic and reconstructive surgery.

New Guidelines Improve Care and Practice Standards for Adults With Hearing Loss
Mar 03, 2023 View All News
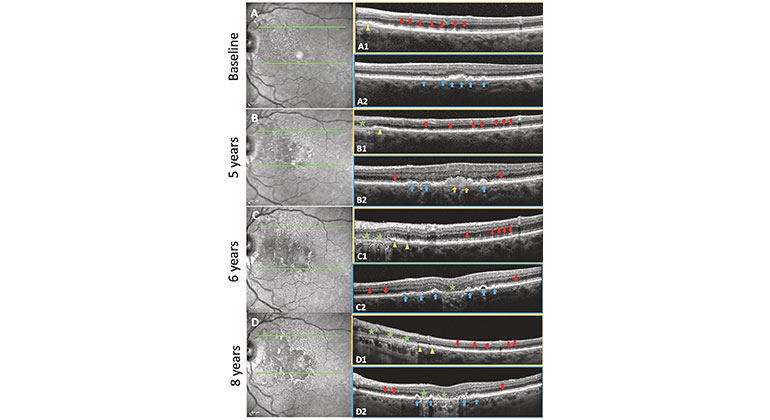
High-Tech Imaging Offers New Way to Detect Signs of Early Glaucoma
Aug 02, 2022 View All News
Mount Sinai’s Alon Harris, MS, PhD, FARVO, Receives Top Honor From The Glaucoma Foundation
Jun 23, 2025 View All NewsMount Sinai Ophthalmologists Develop Novel Protocol to Rapidly Diagnose and Treat Eye Stroke
Feb 13, 2024 View All NewsPatients With Specific Types of Lipids May Be at Higher Risk of Developing Blinding Eye Disease
Jun 13, 2023 View All News
New Guidelines Improve Care and Practice Standards for Adults With Hearing Loss
Mar 03, 2023 View All News
High-Tech Imaging Offers New Way to Detect Signs of Early Glaucoma
Aug 02, 2022 View All News
Mount Sinai’s Alon Harris, MS, PhD, FARVO, Receives Top Honor From The Glaucoma Foundation
Jun 23, 2025 View All NewsMount Sinai Ophthalmologists Develop Novel Protocol to Rapidly Diagnose and Treat Eye Stroke
Feb 13, 2024 View All NewsPatients With Specific Types of Lipids May Be at Higher Risk of Developing Blinding Eye Disease
Jun 13, 2023 View All News