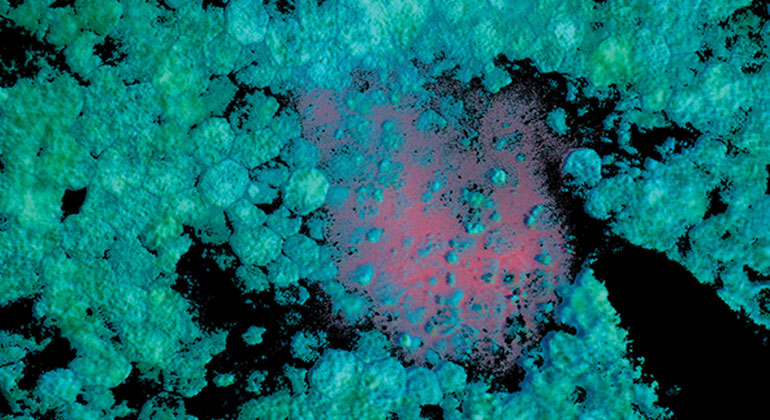
Research and Innovation
At New York Eye and Ear Infirmary of Mount Sinai (NYEE), we are striving daily to uncover the next generation of treatments for a wide range of conditions. Never satisfied with the status quo, our scientists work tirelessly to give patients of today and tomorrow new and better options in terms of medications, surgical techniques, prevention practices, and more.
With resources that include The Shelley and Steven Einhorn Clinical Research Center, the Eye and Vision Research Institute, and the Ophthalmic Innovation and Technology Program, NYEE has the expert talent, imaging facilities, and collaborative infrastructure necessary to learn more about complex diseases and design novel approaches for treating them.
With a wealth of clinical trials available in both ophthalmology, and otolaryngology, our patients have access to the newest available therapies.
Such a strong commitment to research positions NYEE to make great advances in order to achieve the best possible health for patients both here in New York and around the world.
Office of Research Services
Research conducted by Icahn School of Medicine at Mount Sinai faculty, at the New York Eye and Ear Infirmary of Mount Sinai, is subject to Mount Sinai’s ethical and legal requirements for the conduct and oversight of human research. The Office of Research Services (ORS) serves as a central resource for the Mount Sinai Health System research community, and oversight of human subjects research is provided by the Program for the Protection of Human Subjects (PPHS).